This overview details cardiovascular anatomy and physiology‚ essential for understanding the heart’s function․ Resources like Osmosis and SpringerLink offer comprehensive insights into cardiac structures and mechanisms․
Overview of the Cardiovascular System
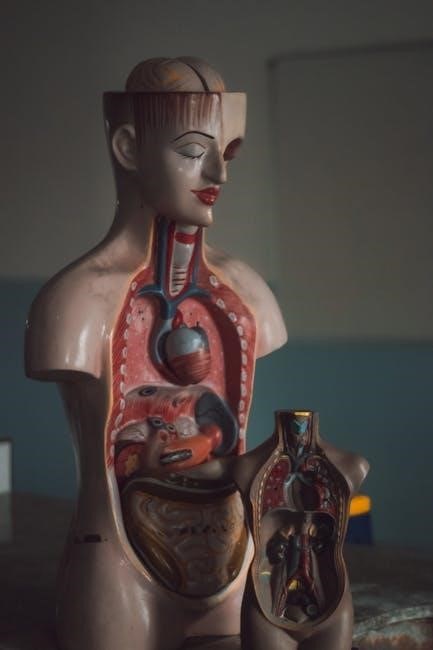
The cardiovascular system‚ at its core‚ is the body’s transport network‚ relentlessly working to deliver oxygen‚ nutrients‚ hormones‚ and immune cells to tissues while removing metabolic waste․ This intricate system fundamentally revolves around the heart – a muscular pump propelling blood throughout the body․ It comprises the heart‚ blood vessels (arteries‚ veins‚ and capillaries)‚ and blood itself․
Arteries carry oxygenated blood away from the heart‚ branching into smaller arterioles and ultimately capillaries where exchange occurs․ Veins then return deoxygenated blood to the heart․ Understanding this circulatory pathway‚ detailed in resources like anatomy and physiology notes and the “Handbook of Cardiac Anatomy‚ Physiology‚ and Devices‚” is crucial․ The lymphatic system‚ often studied alongside‚ plays a vital role in fluid balance and immunity․ Efficient circulation‚ measured by cardiac output (stroke volume x heart rate)‚ is paramount for maintaining homeostasis and supporting all bodily functions․
Importance of Understanding Cardiac Anatomy and Physiology
A robust grasp of cardiac anatomy and physiology is foundational for healthcare professionals‚ enabling accurate diagnosis and effective treatment of cardiovascular diseases․ Comprehending the heart’s structure – chambers‚ valves‚ and layers – is vital for interpreting diagnostic tools and understanding pathological changes․ Resources like Osmosis’s high-yield notes and detailed diagrams are invaluable․
Knowledge of the conduction system‚ from the SA node to Purkinje fibers‚ clarifies arrhythmia mechanisms․ Understanding the cardiac cycle – systole and diastole – explains blood pressure regulation and heart failure․ Furthermore‚ recognizing normal versus abnormal heart sounds (murmurs) aids in clinical assessment․ The carotid sinuses’ role in blood pressure control highlights the interconnectedness of the cardiovascular system․ Essentially‚ a solid foundation in these principles‚ as detailed in comprehensive texts‚ is indispensable for providing optimal patient care and advancing cardiac research․

Structures of the Heart
The heart’s anatomy includes chambers‚ valves (tricuspid‚ mitral‚ pulmonary‚ aortic)‚ and layers (pericardium‚ myocardium‚ endocardium)․ Coronary arteries and veins support its function․
Chambers of the Heart: Atria and Ventricles
The heart comprises four chambers: two atria and two ventricles․ The atria‚ superior chambers‚ receive blood returning to the heart – the right atrium receives deoxygenated blood from the body via the superior and inferior vena cava‚ while the left atrium receives oxygenated blood from the lungs through the pulmonary veins․
These chambers possess relatively thin walls‚ as they primarily function to propel blood into the ventricles․ The ventricles‚ located inferiorly‚ are the primary pumping chambers․ The right ventricle pumps deoxygenated blood to the lungs via the pulmonary artery‚ and the left ventricle‚ with its thicker‚ more muscular walls‚ forcefully ejects oxygenated blood into the aorta for systemic circulation․
This structural difference in ventricular wall thickness reflects the differing pressures required for pulmonary versus systemic circulation․ Understanding these chamber roles is fundamental to grasping cardiac physiology and potential pathologies․
Heart Valves: Tricuspid‚ Mitral‚ Pulmonary‚ and Aortic
The heart’s four valves ensure unidirectional blood flow․ The tricuspid valve‚ positioned between the right atrium and ventricle‚ prevents backflow into the atrium during ventricular contraction․ Similarly‚ the mitral valve (bicuspid) guards the left atrium-ventricle junction․ These atrioventricular valves are anchored by chordae tendineae to the papillary muscles‚ preventing prolapse during pressure changes․

On the outflow side‚ the pulmonary valve controls blood flow from the right ventricle into the pulmonary artery‚ while the aortic valve regulates flow from the left ventricle into the aorta․ These semilunar valves open with ventricular contraction and close during diastole‚ preventing backflow into the ventricles․
Proper valve function is crucial for efficient circulation․ Dysfunction‚ leading to stenosis or regurgitation‚ significantly impacts cardiac output and overall cardiovascular health․ Understanding valve anatomy is key to diagnosing and treating related conditions․
Layers of the Heart Wall: Pericardium‚ Myocardium‚ Endocardium
The heart wall comprises three distinct layers․ The outermost pericardium‚ a double-layered sac‚ protects the heart and reduces friction with a fluid-filled space․ Its fibrous and serous layers provide both structural support and lubrication during contractions․
The middle and thickest layer‚ the myocardium‚ is composed of cardiac muscle responsible for the heart’s pumping action․ Its contractile fibers‚ arranged in spiral and circular patterns‚ enable efficient ejection of blood․ The myocardium’s thickness varies based on chamber function and workload․
Finally‚ the innermost endocardium‚ a thin layer of epithelial cells‚ lines the heart chambers and covers valves․ It minimizes friction as blood passes through‚ contributing to smooth blood flow․ This layer is continuous with the blood vessels‚ ensuring seamless circulation․ Understanding these layers is fundamental to comprehending cardiac physiology and pathology․
Coronary Circulation: Arteries and Veins
The heart’s function relies on its own dedicated blood supply – the coronary circulation․ Coronary arteries branch from the aorta‚ delivering oxygenated blood to the myocardium․ The left and right coronary arteries‚ and their major branches‚ ensure adequate perfusion of all heart regions․
These arteries create a network of capillaries within the heart muscle‚ facilitating oxygen and nutrient exchange․ Deoxygenated blood is then collected by cardiac veins‚ which converge into the coronary sinus – a large vein on the heart’s posterior surface․
The coronary sinus empties directly into the right atrium‚ returning blood to the pulmonary circulation for re-oxygenation․ Efficient coronary circulation is vital; blockages can lead to ischemia and potentially‚ myocardial infarction․ Understanding this system is crucial for diagnosing and treating heart conditions․

Conduction System
The heart’s intrinsic conduction system initiates and coordinates contractions․ Key components include the SA node‚ AV node‚ Bundle of His‚ and Purkinje fibers‚ ensuring rhythmic function․

Sinoatrial (SA) Node: The Heart’s Pacemaker
The Sinoatrial (SA) node‚ often termed the heart’s natural pacemaker‚ is a specialized cluster of cells located in the right atrium’s wall․ This node initiates the electrical impulses that trigger each heartbeat‚ setting the rhythm for the entire cardiac cycle; Its inherent automaticity allows it to depolarize spontaneously and consistently‚ generating approximately 60-100 impulses per minute at rest․
These impulses then spread throughout the atria‚ causing them to contract․ The SA node’s rate is modulated by the autonomic nervous system; sympathetic stimulation increases heart rate‚ while parasympathetic stimulation decreases it․ Understanding the SA node’s function is crucial‚ as disruptions can lead to arrhythmias․ Resources like those found on Osmosis and within the Handbook of Cardiac Anatomy‚ Physiology‚ and Devices emphasize its central role in maintaining cardiovascular homeostasis․ Proper SA node function is paramount for efficient blood circulation․
Atrioventricular (AV) Node and Bundle of His
Following impulse generation in the SA node‚ the Atrioventricular (AV) node receives and briefly delays the signal․ This delay‚ crucial for coordinated atrial contraction before ventricular contraction‚ occurs within the AV node located between the atria and ventricles․ The AV node also serves as a backup pacemaker if the SA node fails‚ though at a slower rate․
From the AV node‚ the impulse travels down the Bundle of His‚ a specialized conduction pathway dividing into left and right bundle branches․ These branches extend along the interventricular septum‚ ultimately leading to the Purkinje fibers․ This pathway ensures rapid and synchronized ventricular depolarization and contraction․ Resources detailing cardiac anatomy and physiology‚ such as those available through SpringerLink and Osmosis‚ highlight the AV node and Bundle of His’s vital role in efficient cardiac output․ Any disruption to this pathway can cause significant arrhythmias․
Purkinje Fibers: Distribution and Function

The Purkinje fibers represent the terminal branches of the cardiac conduction system‚ originating from the Bundle Branches and spreading throughout the ventricular myocardium․ These fibers are characterized by their large diameter and rapid conduction velocity‚ enabling near-simultaneous depolarization of ventricular muscle cells․
Their extensive distribution ensures coordinated ventricular contraction‚ maximizing ejection fraction and cardiac output․ Unlike typical cardiac muscle cells‚ Purkinje fibers have fewer myofibrils‚ contributing to their faster conduction speed․ They penetrate the ventricular walls‚ terminating just before reaching the ventricular muscle cells‚ facilitating efficient signal transmission․ Understanding their distribution and function is crucial when studying cardiac anatomy and physiology‚ as detailed in resources like Osmosis and SpringerLink․ Damage to Purkinje fibers can lead to arrhythmias and impaired ventricular function‚ highlighting their critical role in maintaining a regular heartbeat․

Cardiac Physiology
Cardiac physiology encompasses the heart’s mechanical and electrical functions‚ including the cardiac cycle‚ stroke volume‚ and cardiac output—vital concepts explored in detailed anatomy and physiology resources․
Cardiac Cycle: Systole and Diastole
The cardiac cycle represents the complete sequence of events occurring during one heartbeat․ It’s fundamentally divided into two primary phases: systole and diastole․ Systole signifies the contraction phase‚ where the ventricles forcefully eject blood into the pulmonary artery and aorta․ This is driven by coordinated muscle fiber shortening․
Conversely‚ diastole represents the relaxation phase‚ allowing the ventricles to fill with blood returning from the atria․ This filling is crucial for preparing for the next contraction․ Both atria and ventricles experience systole and diastole‚ but they occur at slightly different times to optimize blood flow․
Understanding these phases‚ alongside the interplay of valves and pressure gradients‚ is central to grasping cardiac function․ Resources detailing anatomy and physiology‚ such as those found on Osmosis and in the Handbook of Cardiac Anatomy‚ Physiology‚ and Devices‚ provide detailed illustrations and explanations of this cyclical process․
Stroke Volume and Cardiac Output
Two key measures of cardiac performance are stroke volume (SV) and cardiac output (CO)․ Stroke volume defines the amount of blood ejected by the left ventricle with each contraction – essentially‚ the ‘volume’ of each ‘stroke’․ It’s influenced by factors like preload‚ afterload‚ and contractility․

Cardiac output‚ however‚ represents the total volume of blood pumped by the heart per minute․ It’s calculated by multiplying stroke volume by heart rate (CO = SV x HR)․ This value provides a comprehensive assessment of the heart’s ability to meet the body’s circulatory demands․
Variations in either stroke volume or heart rate directly impact cardiac output‚ allowing the heart to adjust to changing physiological needs‚ such as exercise or stress․ Understanding these parameters‚ as detailed in resources like Osmosis and the Handbook of Cardiac Anatomy‚ Physiology‚ and Devices‚ is vital for evaluating cardiovascular health․
Regulation of Heart Rate: Autonomic Nervous System
The heart’s rate isn’t metronomic; it’s dynamically regulated by the autonomic nervous system (ANS)․ This system comprises the sympathetic and parasympathetic branches‚ exerting opposing influences․ The sympathetic nervous system‚ via norepinephrine release‚ generally increases heart rate and contractility – preparing the body for ‘fight or flight․’
Conversely‚ the parasympathetic nervous system‚ primarily through the vagus nerve releasing acetylcholine‚ decreases heart rate‚ promoting a ‘rest and digest’ state․ This balance ensures appropriate cardiovascular responses to diverse physiological demands․
Baroreceptors‚ located in carotid sinuses‚ play a crucial role‚ detecting blood pressure changes and relaying information to the ANS․ Resources like those found on Osmosis and within the Handbook of Cardiac Anatomy‚ Physiology‚ and Devices‚ detail these intricate regulatory mechanisms‚ vital for maintaining circulatory homeostasis․
Clinical Relevance
Understanding normal and abnormal heart sounds‚ alongside carotid sinus function‚ is crucial for diagnosing cardiovascular conditions‚ as detailed in resources like Osmosis and SpringerLink․
Normal Heart Sounds
Normal heart sounds‚ often described as “lub-dub‚” are fundamental to assessing cardiac health․ These sounds are primarily caused by the closure of the heart valves during the cardiac cycle․ The first heart sound‚ “lub‚” signifies the closing of the mitral and tricuspid valves at the beginning of ventricular systole․ This is a relatively lower-pitched and longer sound․
Subsequently‚ the second heart sound‚ “dub‚” represents the closure of the aortic and pulmonary valves‚ marking the start of ventricular diastole․ This sound is typically higher-pitched and shorter in duration․
These sounds are best auscultated with a stethoscope at specific anatomical locations on the chest‚ allowing clinicians to correlate the sounds with valve function and chamber activity․ Understanding the timing and characteristics of these sounds‚ as detailed in resources like Osmosis and the Handbook of Cardiac Anatomy‚ Physiology‚ and Devices‚ is essential for differentiating them from abnormal sounds․
Abnormal Heart Sounds (Murmurs)
Cardiac murmurs represent abnormal heart sounds‚ often indicative of turbulent blood flow․ Unlike the clear “lub-dub” of normal heart sounds‚ murmurs present as whooshing or blowing sounds during systole or diastole․ These can arise from various causes‚ including valve stenosis (narrowing) or regurgitation (leaking)‚ congenital heart defects‚ or increased blood flow․
Murmurs are graded on a scale of 1 to 6 based on their intensity‚ with higher grades indicating louder murmurs․ Their characteristics – timing‚ location‚ radiation‚ pitch‚ and quality – are crucial for diagnosis․
Resources like the Handbook of Cardiac Anatomy‚ Physiology‚ and Devices and educational platforms such as Osmosis emphasize the importance of careful auscultation and correlation with patient history to determine the underlying cause of a murmur․ Identifying murmurs is a key skill in assessing cardiovascular health and guiding appropriate clinical intervention․
Carotid Sinuses and Blood Pressure Regulation
Located near the base of the carotid arteries‚ the carotid sinuses contain baroreceptors – specialized nerve endings sensitive to changes in blood pressure․ These receptors play a vital role in maintaining cardiovascular homeostasis by providing feedback to the brainstem’s cardiovascular control center․
When blood pressure rises‚ baroreceptors increase their firing rate‚ signaling the brainstem to decrease heart rate and cause vasodilation‚ thus lowering blood pressure․ Conversely‚ a drop in blood pressure reduces firing‚ prompting an increase in heart rate and vasoconstriction to elevate pressure․
Understanding the function of carotid sinuses‚ as detailed in resources like Osmosis’s cardiovascular anatomy and physiology notes‚ is crucial for comprehending blood pressure regulation․ Disruptions to this system can lead to conditions like orthostatic hypotension or contribute to hypertension․

Leave a Reply